As an increasing number of people across the country get tested for COVID-19 antibodies, health experts are cautioning that much is still unknown about what the results mean — including if antibodies provide protection from catching the virus again, how strong that protection might be and how long it may last.
A COVID-19 antibody test, also known as a serology test, aims to detect the presence of antibodies in the blood specific to SARS-CoV-2, the virus that causes COVID-19.
A positive test result is presumed to mean that a person was exposed to the virus at some point in the past and their immune system produced proteins called antibodies to fight it off. The tests are different from nasal swab tests and do not indicate whether a person is currently infected with the virus.
The Centers for Disease Control and Prevention, in a June 30 update, said it does not know if people who recover from COVID-19 can get infected again. It also said even with a positive test for antibodies, people “still should take preventive measures to protect yourself and others.”
[sc:text-divider text-divider-title=”Story continues below gallery” ]
Dr. Raymond Kiser, medical director of hospital care physicians at Columbus Regional Health, said antibody testing is “probably not that helpful” for most people because it won’t tell them if a particular bout of illness in the past was COVID-19 or if they are currently immune to the virus.
Additionally, Kiser said he is “nervous” that people who test positive for COVID-19 antibodies may be lulled into a false sense of security and “think they’re protected and they may not be.”
“We have no idea if you develop (COVID-19) antibodies, does that confer immunity, and if it does, for how long,” he said. “…When people ask me, ‘Should I get antibody tested,’ in all honesty, I usually tell them no. It’s not going to answer the question you really want to know and that is ‘Are you protected from this virus?’ And the answer is, ‘I don’t know’ — even if you have antibodies I won’t know the answer to that.”
Studies underway
Currently, numerous studies are underway to better understand the protective role of antibodies against the novel coronavirus, but just months into the pandemic much still remains unknown.
Health experts say antibodies usually confer at least partial immunity against some viruses, but length and level of protection varies.
The antibodies produced in response to an infection of certain viruses, like the one that causes measles, are believed to provide lifetime immunity, while antibodies generated against other viruses, like the ones that cause the common cold, tend to offer shorter-lived protection. For some viruses, however, antibodies provide nearly no protection at all.
Most health experts, including Kiser, suspect that COVID-19 antibodies may offer some level of protection against the virus in the short-term, but nobody knows for sure where those antibodies fall on the spectrum.
The strongest evidence so far for short-term immunity comes from a study done on monkeys infected with the novel coronavirus, and it’s not yet clear the extent to which those results will hold true for humans, Kiser said.
“The only data that we really have for that is a study done on primates where they actually exposed them to the SARS-CoV-2 virus and those who had antibodies didn’t get re-infected at 30 days. But we don’t really know if that applies to humans,” Kiser said.
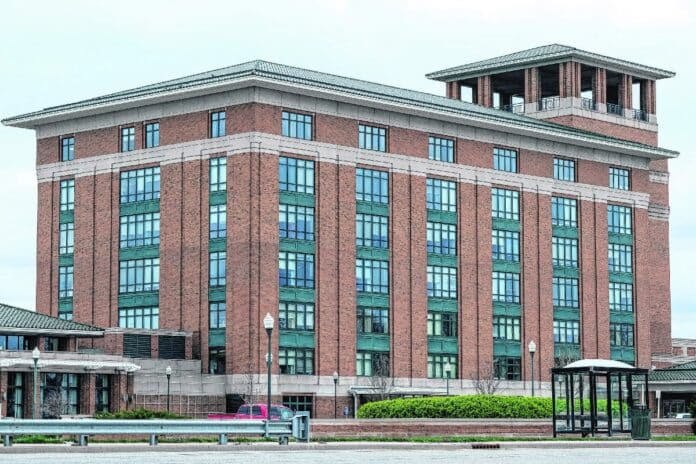
CRH, for its part, does have COVID-19 antibody tests in-house, hospital officials said.
As of mid-July, CRH had administered 106 antibody tests, but only one of them had come back positive, Kiser said.
In June, the U.S. Food and Drug Administration released performance results of 21 antibody tests, including the Siemens Healthineers total antibody test, which is the antibody test that CRH uses, according to hospital officials.
The FDA started requiring companies to submit testing data and apply for emergency authorization to remain on the market in May after reports of faulty results and fraud emerged, The Associated Press reported.
The accuracy of antibody tests is measured by their “sensitivity,” or their ability to identify if someone has COVID-19 antibodies in their blood, and their “specificity,” which is their ability to determine who does not have the antibodies, according to the FDA.
The tests are also described by their positive predictive value, which measures how likely it is that a person who receives a positive result from a test truly has COVID-19 antibodies based on the test’s sensitivity, specificity and assumptions about the prevalence of the virus in a community, according to the FDA.
“Every test returns some false positive and false negative results” and some people may need more than one antibody test to ensure accurate results, according to the FDA’s website.
The test CRH uses was shown to be 100% sensitive and 99.8% specific and has a positive predictive value of at least 96.5% depending on how prevalent the virus is in a given community, according to the FDA’s performance data.
That means that the test is expected to correctly identify the presence of COVID-19 antibodies at least 96.5% of the time, according Siemens Healthengineers.
“We have not seen a lot of positive (antibody) testing here so far,” Kiser said. “With regards to the tests, especially the ones that we are using, we do believe that they are very specific, which means that if you have this antibody positive it means that you’ve definitely been exposed to the SARS-CoV-2 virus.”
Public health efforts
Though the protective role of antibodies against COVID-19 isn’t clear, antibody testing could provide valuable information for public health efforts, including studies seeking to determine how many people in a community have been exposed to the virus.
Researchers across the United States, including in Indiana, have embarked on such studies, aiming to use a representative sample of the overall population to shed light on the prevalence of COVID-19 in different areas of the country.
The hope, health experts say, is that these studies may help scientists and doctors measure the infection fatality rate of COVID-19, or the proportion of deaths from the virus compared to the total number of people diagnosed with the disease.
So far, initial results from several studies have found varying degrees of COVID-19 prevalence across the United States.
A study by the University of Southern California and the Los Angeles County Health Department found in May that an estimated 2.5% to 7% of adults in Los Angeles County had contracted the new coronavirus in May.
A similar study conducted by Massachusetts General Hospital and the Boston Public Health Commission found that roughly 10% of Boston residents tested positive for COVID-19 antibodies in May.
The prevalence of COVID-19 in Indiana, however, is believed to be much lower.
Last month, researchers at the Indiana University Richard M. Fairbanks School of Public Health at IUPUI and the Indiana State Department of Health released preliminary data from the second phase of their prevalence study, finding that a total of 1.5% of participants tested positive for COVID-19 antibodies, up from 1.1% in the first phase, according to preliminary findings.
“One of the big things we want to know about this virus is how many people have been infected,” Kiser said. “…If I know how many people in a general population have been exposed and I know how many people have died, then I can really tell you the information that you’re going to want to know, which is if everybody gets exposed, how many deaths can we expect?”
Scientists are getting closer to an answer, according to leading science journal Nature. Research so far suggests that COVID-19 is five to eight times deadlier than the seasonal flu, which kills hundreds of thousands of people around the world each year.
The seasonal flu has an infection fatality rate of around 0.1%, meaning that one out of every 1,000 people infected would be expected to die, Kiser said. By comparison, five to eight out of every 1,000 people infected with the SARS-CoV-2 virus would be expected to die.
In other words, if all of Indiana’s estimated 6.7 million residents were to be infected with COVID-19, an estimated 33,500 to 53,600 people would be expected to die, compared an estimated 6,700 estimated deaths from influenza.
“Influenza is probably one of our No. 1 infectious killers in the U.S., and this thing is five to eight times worse,” Kiser said.
In addition, antibody testing could help identify potential blood plasma donors for convalescent plasma therapy, which is an experimental treatment for COVID-19 currently in trials at numerous hospitals across the country, including Columbus Regional Hospital, where at least 54 patients have received the treatment, Kiser said.
Convalescent plasma therapy involves giving COVID-19 patients an infusion of blood plasma from people who have already recovered from the illness, CRH officials said.
Though it currently is not known precisely how COVID-19 antibodies work, researchers and doctors believe that plasma from COVID-19 survivors could boost the immune system’s response in a patient whose body is struggling to fight off the infection.
At this point, however, antibody testing is most useful for public health efforts and identifying potential plasma donors, Kiser said.
“Right now, the best use of antibody testing is public health,” Kiser said. “…I think on an individual basis, it’s probably not that helpful.”
[sc:pullout-title pullout-title=”Where to learn more” ][sc:pullout-text-begin]
Anyone with concerns about COVID-19 is urged to call the health system’s Triage Resource Call Center, a phone resource line launched by CRH to handle calls from residents with questions and concerns about exposure or symptoms associated with COVID-19. The phone line is open daily from 7 a.m. to 8 p.m. and is staffed by registered nurses who will offer screening questions and potentially recommend a course of action for patients.
The phone resource line can be contacted at 812-379-4449.
Visit crh.org/news/2020/03/16/coronavirus-update-what-you-need-to-know for more information.
Visit the Community COVID-19 Task Force’s website at covid19communitytaskforce.org.
[sc:pullout-text-end]




